|
|
||||||||||||||
|
Radiotherapy |
|
|||||||||||||
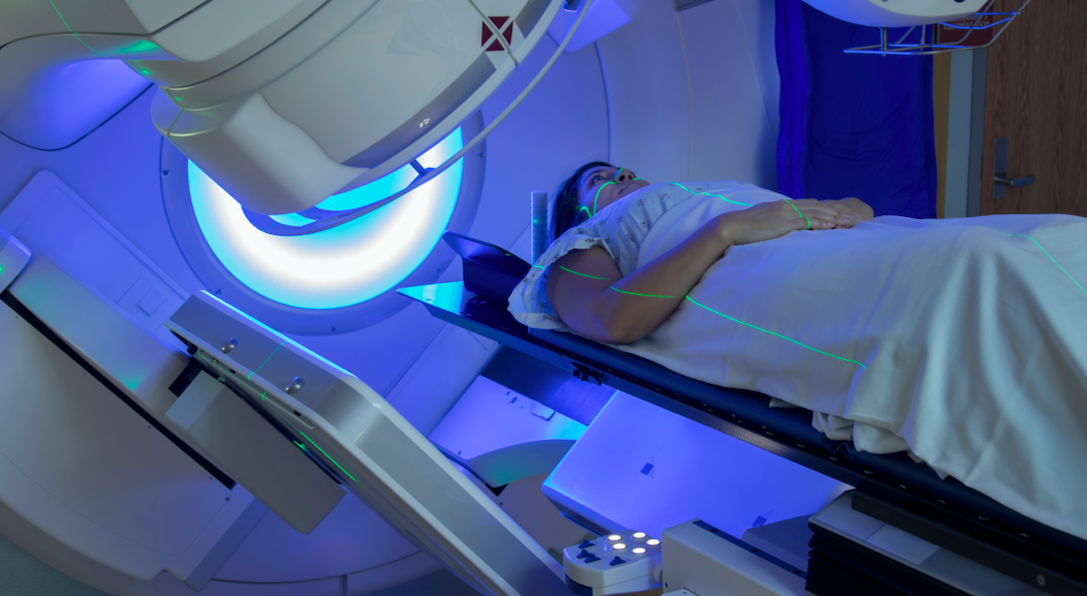
What is radiotherapy The use of high energy x-rays to treat patients with malignant disease. Radiotherapy beams can be directed very accurately to any area of the body using highly sophisticated machines. The most commonly used of these are called a linear accelerator, with other machines called orthovoltage or superficial depending on the energy of the X-rays required. The technology behind radiotherapy delivery is improving rapidly. The majority of radiotherapy treatments originate from machines called linear accelerators. These are large and sophisticated which produce high energy x-rays (or photons). The are also expensive and require a lot of highly trained manpower to keep them working accurately. The head of the machine, bed and gantry can be rotated and moved in multiple directions to ensure the radiotherapy beam can enter the body in virtually any direction. In the passed the beam only came out in square shapes. Conformal
radiotherapy. This is now routine technology available in the vast
majority of radiotherapy centres throughout the world. Lead blocks or This is an example of a patient with cancer of the air sinuses of the face. The green line is shape of the beam coming out of the linear accelerator but the purple line is eventual shape after it has been modified by the lead blocks in order to conform the shape of the target. In this case, this has avoided irradiating the eyes which may course cataract and dryness later in life and the salivary glands causing an uncomfortable dry mouth. Virtually all linear accelerators in clinical practice are now capable of conformal radiotherapy. Not all machines are capable of two further recent scientific developments: Intensity modulated radiotherapy (IMRT) The next generation of machines are even more accurate, capable of varying the intensity of the beam within the area treated area. In this way, the contours of the body are taken into account avoiding hot and cold spots within the treated field. This is not optimal as the hot spots could damage the normal skin causing fibrosis and pain. On the the other hand the cold spots could not kill the cancer cells in this area allowing it to not be locally controlled and increase the risk of it returning after treatment or spreading to another part of the body. Tomotherapy At the time of writing this page (Feb 2009) there are only two tomotherapy machine sin the UK (Addenbrooke's Hospital Cambridge and the Cromwell hospital, London). These are the most sophisticated machines commercially available They are capable of changing the both the shape and intensity of the beam during the actual treatment. As a result they can produce a very accurate distribution of radiotherapy in the body. In stead of 2-4 beams it tend to use multiple constantly changing beams. This machine is enabling doctors to treat tumours which previously were not possible due to their proximity to other vital organ which can now be protected. They also have more accurate image guidance systems. Image guided radiotherapy (IGRT). Normally the radiotherapy beam is "set up" to the correct position using tattoos on the skin or marks on a shell. Although generally accurate, errors can be made if the skin is loose or moves due to breathing or changes in shape of the patient. Sometime the target organ or cancer can move during the treatment. A good example of this is the bladder depending how much urine it contains or the prostate which can move depending how much gas or feaces there is in the rectum. IGRT uses a technique which guides the radiotherapy using a target within the cancer or organ itself so it doesn't matter so much if it has moved between days of treatments. Several techniques are used for this including CT imaging on the linear accerator itself or the insertion of a gold grain for example in the prostate before treatment. Proton beam radiotherapy: This is a type of radiotherapy that uses a beam of high energy protons, which are small parts of atoms, rather than high energy x-rays (called “photons”) to treat specific types of cancer. Proton beam therapy enables a dose of high energy protons to be precisely targeted at a tumour, reducing the damage to surrounding healthy tissues and vital organs which is an advantage in certain groups of patients or where the cancer is close to a critical part of the body such as the spinal cord. It is only suitable for certain types of cancer, such as highly complex brain, head and neck cancers and sarcomas as it does not lead to better outcomes for many cancer cases than using high energy x-rays, which is still considered the most appropriate and effective treatment for the majority of cancers. Like high energy x-ray radiotherapy, proton beam therapy is painless, but patients may experience side effects similar to those experienced from other forms of radiotherapy.Two NHS centres will provide high energy proton beam therapy in the UK, The Christie NHS Foundation Trust (Manchester) and University College London Hospital (UCLH) NHS Foundation Trust. Traveling: The equipment necessary to administer radiotherapy is expensive, and requires a lot of space and specially trained staff, radiotherapy departments tend to be found in the larger regional hospitals or cancer centres. Therefore if you do require radiotherapy you probably have to do a lot of traveling each day. in some centres their are hostels or local accommodation. Other types of Radiotherapy. Radiotherapy can also be delivered to small volumes of the body by implanting radioactive wires or seeds, sometimes called brachytherapy or low dose rate radiotherapy which produce gamma rays. Radioisotopes can also ne injected into the body, for example for the treatment of thyroid cancer. Why have radiotherapy? The indications for radiotherapy are broadly divided into two main categories, palliative or radical. It should have been explained which category applies to you. Palliative means that radiotherapy is given to relieve local symptoms from a tumour, for example to lessen pain, or stop bleeding, or to prevent damage to neighboring structures such as nerves. It is usually given over a short period of time, either on one day or one or two weeks. Radical radiotherapy aims to curative or improve the chances of cure. In this case a higher dose of radiotherapy is given aiming to completely eradicate the tumour within the irradiated field. This has to be spread over a longer period, often four to seven weeks, to allow your normal cells to repair between fractions enabling a better therapeutic ratio (more cancer cells killed and less damage to the normal tissues). What happens when you have radiotherapy? You would have had a consultation with an oncologist who specialises in radiotherapy who would have arranged for the radiotherapy which may be in your current hospital or a different hospital with radiotherapy equipment. Before treatment you will be asked to sign a consent form. The main object of this form is to clarify that patients fully understand the treatment and are aware of any potential side effects. The risk of side effects do depend on whether you having treatment to the breast alone or the breast and armpit. These side effects are broadly split into early effects, which can come on during or shortly after radiotherapy but are temporary, and late effects which can be long term. Your oncologists will have carefully taken these into account when considering the benefits of treatment and will inform you of the side effects you are most likely to get. Let us now describe some of these side effects but it must be stressed that what follows is a general overview of treatment - you may well not experience any of these effects and it is possible you may experience others not mentioned at this initial consultation. Your first appointment at the radiotherapy centre will usually a planning session. On arrival in the department patients should report to the reception desk, show them their appointment card, and will directed to the clinic rooms, CT scanner or simulator. The simulator is a direct mock-up of an actual therapy machine, but the x-rays produced are only for pictures. This helps the doctor decide the exact area within the body that needs treatment. In most cases, patients are planned on a computer on the images taken on the designated CT scanner. These scans are required to plan the radiotherapy of some areas of the body. For patients receiving radiotherapy to the head or neck it may be directed to the mould room where a plaster cast impression is taken. - see having a mould During your visits to the radiotherapy centre you will encounter members of staff called radiographers. These are people who operate the machines to plan and give you your treatment. They work closely with the doctors and other people within the department. They can give you help and advice about any aspect of your treatment, and don't be embarrassed to ask them anything you are concerned or anxious about.
Once all the measurements are taken, the rest of the treatment planning will be behind the scenes with the aid of a physicist who is a highly trained specialist in the subject of radiation. They assists the oncologist in deciding the best way of delivering the amount of radiotherapy needed. Only when the radiographers, physicist, and doctors are one hundred percent confident with your planned treatment will patients proceed to treatment. The treatment machine looks like the simulator,
but it is a lot bigger. Patients are not required to do anything that they've not already
done in the simulator. Treatment usually lasts one or two minutes, and while the machine
is on they usually do not have any sensation. Even though the radiographers are not in the
room while they are being treated, they are being watched at all times on a video camera.
There is also an intercom, which is left on so they can hear as well as see you
constantly. If patients feel any distress during treatment, the machine can be turned off
and the radiographers will be at their side within seconds. Having a mould. This applies only if you are having radiotherapy to the head and neck area. Often in this situation a shell or mask in made of clear plastic and will cover your head and face during treatment. Holes will be cut for your eyes, nose and mouth and the mask will fix on to the treatment table top. Radiotherapy treatment requires you to be positioned precisely in the radiotherapy beam. You also need to keep very still during treatment.
Extra
visits to the radiotherapy department are required to complete a mask or shell. Firstly, we need to take an
impression of the
Taking an
impression can be a little messy, so we suggest that you wear clothes that can
easily be removed or loose clothing with a low collar. It is important that the shell fits well during your treatment. The
following points will help the she to fit properly;
During standard radiotherapy your skin may get red and itchy, similar to sunburn. Your radiographers will be looking for these reactions, but you should let them know as soon as you feel soreness. Do not apply creams or dressings, unless recommended by your radiographer or oncologist. Avoid sun, excessive washing, and rubbing on these areas. Each department will have its own skin care policy, which will be available to you. If the ovaries in women, or the testes in men, are being irradiated, there will be a risk of infertility and reduced hormone output which should have been discussed with you in advance. On no account must a female patient be pregnant, but there is no risk of harming any babies or pregnant women if you meet them during your radiotherapy course or afterwards. Radiotherapy to your mouth and throat will cause some soreness (otherwise called mucositis). This usually starts halfway through your treatment, and is at its worst towards the end of treatment, but can persist for some time afterwards. It is important to keep your mouth clean, with regular soft tooth brushing, dental floss, and mouth washing. Once mucositis has started, treatment to prevent secondary thrush infection is often given. It is also important to maintain a good nutrition, and avoid smoking and alcohol. With radiotherapy you will lose hair within the treatment area. It usually begins to fall out after two or three weeks. Most hair loss is temporary, but can be permanent in some cases. There are many other acute side effects which have not been mentioned here, but these should have been explained to you before the start of treatment. Late side effects are those which can develop months or even years after the end of radiotherapy. These are the ones your oncologist worries about most. The type of side effect will obviously depend upon which area you are having irradiated. For example, if your salivary glands are irradiated, you will get dryness of the mouth which can last several months after treatment and may be permanent. This side effect in particular should have been discussed with you before starting treatment. Other late side effects are rare, but can cause considerable distress. These include :-
Your oncologist will have taken the risks of these late side effects into account when deciding on your treatment strategy. In any case, the risk is usually no more than one to five percent. These risks should have been discussed with you during your consent consultation. |
||||||||||||||
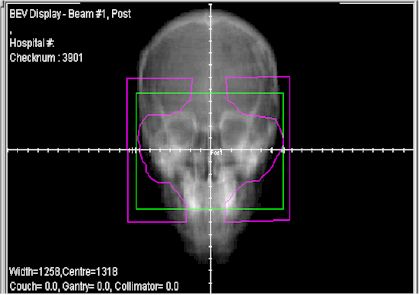 multiple leaves
are put into the beam. This
affectively conforms the shape of the beam into the shape of the tumour, hence
the term conformal radiotherapy.
multiple leaves
are put into the beam. This
affectively conforms the shape of the beam into the shape of the tumour, hence
the term conformal radiotherapy. During this planning stage very
accurate measurements will be taken of the body, and it does require people to be
lying on a fairly hard couch, which may be slightly uncomfortable. In some cases a small
tattoo about the size of a pinhead is made, giving a permanent record of the measurements.
This is probably the longest time patients have to lie on a couch.
During this planning stage very
accurate measurements will be taken of the body, and it does require people to be
lying on a fairly hard couch, which may be slightly uncomfortable. In some cases a small
tattoo about the size of a pinhead is made, giving a permanent record of the measurements.
This is probably the longest time patients have to lie on a couch.