A dry mouth can be a distressing side effect of cancer treatments and if prolonged
can lead to pain and soreness. A dry mouth can lead to secondary infection and
bleeding. Lack of saliva then causes difficulty swallowing as it is hard to chew
food and form a bolus. A dry mouth also causes problems with speech as the
tongue tends to stick to the side or roof of the mouth. This page describes the
common causes of a dry mouth during or after cancer treatments and suggests some
practical tips which may help.
Common causes of
a dry mouth:
-
Mouth breathing e.g. a blocked nose
-
Painkillers - opiates, codeine
-
Antisickness - hyoscine
-
Antidepressants or amtitrypiline
-
Damage to the salivary glands - particularly after
radiotherapy to the head and neck area
-
After prolonged chemotherapy regimens, saliva production can temporarily reduce
-
Dehydration from any cause
-
High calcium in blood stream (hypercalcaemia)
-
Previous medical conditions e.g. autoimmune diseases affecting the gland
Tips for a dry mouth
Good mouth
care when you have a dry mouth can help to keep the mouth clean, moist and
comfortable. It is especially important to take good care of your mouth while
you are receiving treatment: Careful attention to mouth care will help reduce
the risks of infection and the following instructions are designed to help you
keep your mouth clean and comfortable. If a dry mouth becomes inflamed this is
called oral mucositis often can be painful, and this in turn can make it
difficult to eat and drink.
Clean teeth thoroughly but gently
after each meal and before going to bed. If the gums are delicate it is better
to use a soft toothbrush (baby/infant).
Brand name antibacterial mouthwashes
such as Corsodyl may be used but are quite strong and may damage the fragile
lining of your mouth whilst on treatment. Check with nursing staff for further
advice.
Saline mouthwashes are recommended
if tolerable; 5 mls salt: 500 mls tepid water; (1 tsp. salt: one pint tepid water).
If you are suffering from a mark dry mouth, this supervising doctor needs to be
told, otherwise, the following suggestions may help:
- Have
frequent drinks, even just a few sips at a time to keep your mouth moist.
Fizzy drinks may be most refreshing
- Avoid alcohol or smoking
- Try
sucking ice cubes/ice lollies (these can be flavoured with cordials, fruit
juice or juice based supplements
- Try
making home-made lollies or in the freezer using fruit juice and/or
supplements
- Moisten
food with lots of gravy or
sauces, butter, custard, cream
- Some
people report that chocolate and pastry stick to the roof of the mouth-avoid
them if they do
- Try
sucking sugar free boiled sweets, fruit drops/pastilles, chewing gum or try eating
pineapple chunks or grapefruit segments to increase saliva flow
- Artificial
saliva preparations are available and can be prescribed by your doctor if
felt appropriate
- Use
a mouthwash and brush your teeth regularly
- Keep
lips moist with lip balm
-
Avoid wearing denture
It may be necessary to change the diet to foods
which are soft and moist. Also if there are signs of secondary infection
further treatment may be needed.
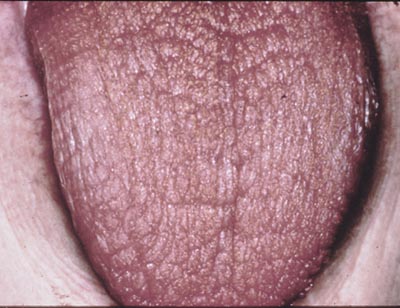
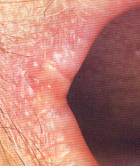
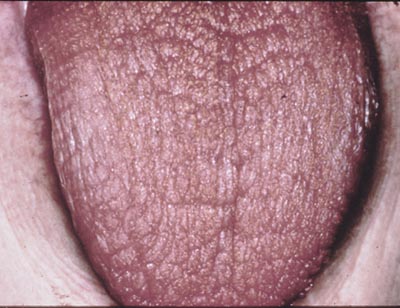
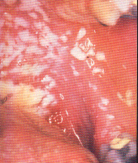
Signs of infection in the mouth: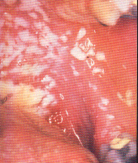
-
red areas
-
pain and swelling
-
blisters
-
white spots
-
coated
tongue
-
bleeding
 Treating a painful mouth Treating a painful mouth
-
Treat infection
- Fundal (candida) with
antifungals such as fluconazole
-
Saline mouthwashes (see above) - Use
two tablets in tepid water, swill around the mouth for two to three minutes but
do not swallow. Useful before meals but it is best not to eat or drink anything
for 10 minutes after using the mouthwash, to gain maximum effect from it. May be
used frequently during the day, provided they are not swallowed.
-
Soluble Paracetamol mouthwash/gargle.
-
Sore lips may be helped with Paracetamol mouthwash.
-
Vaseline is also useful to prevent dryness and cracking.
- Oral barrier gels (e.g.gelclair)
- Painkilling brand name mouthwashes, e.g. Difflam may be useful but please check
with nursing staff before using as some consultants prefer not to prescribe
them
-
In some cases you will be
advised to suck ice/ice-lollies immediately prior to and during
chemotherapy. This is to reduce damage from certain drugs.
|
 Treating a painful mouth
Treating a painful mouth